What Tests Detect Pericardial Effusion?
Pericardial effusion is a condition in which there is an excessive accumulation of fluid between the heart and the pericardium. The latter is the sac that covers the heart. Spillage occurs when the liquid exceeds 50 ml. What medical tests can detect pericardial effusion?
There is always a thin layer of fluid between the heart and the pericardium. When you have an illness or injury, this area can become inflamed. The amount of fluid increases. Despite this, you can sometimes have a pericardial effusion without prior inflammation.
The pericardial effusion presses on the heart and affects the way it works. If left untreated, it can cause heart failure and lead to death. Read this article to find out which tests detect a pericardial effusion.
What tests detect pericardial effusion?
Echocardiogram
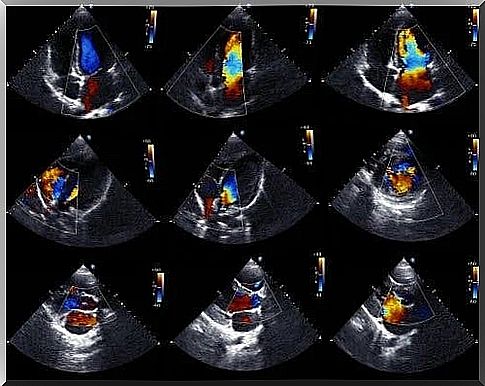
Echocardiogram is the preferred test to detect a pericardial effusion. It is also called echocardiography or cardiac ultrasound and is a test that allows doctors to see the structure of the heart and study its ability to pump blood.
Doppler echocardiogram allows doctors to determine the exact rate of blood flow in the heart. From a technical point of view, the two-dimensional M-mode echocardiogram is the ideal technique for diagnosing, quantifying and monitoring pericardial effusion.
The absence of echoes between the epicardium and the lateral pericardium allows doctors to diagnose pericardial effusion. Then, cardiologists determine the size of the effusion based on the space between the two layers of the pericardium.
We must mention that there are two types of echocardiogram. There is the transthoracic option, in which a device is placed on the chest, above the heart and emits sound. In the case of the transesophageal option, the device is inserted into the digestive tract up to the esophagus. This method provides more detailed information.
The electrocardiogram records the electrical activity of the heart. Basically, it allows doctors to assess heart rate and function. Pericardial effusion causes changes in the chart, but these are not specific.
In general, doctors may see certain abnormalities in the QRS complex. This is a vector that reflects the sum of all electrical discharges that occur in ventricular cells. In general, when there is a pericardial effusion, doctors may notice a reduction in QRS blood pressure.
They may also notice a flattening of the T waves. If the spill is very severe and there are blockages, they may notice an electrical alternation. Usually, the P wave appears wide and bimodal, suggesting an anomaly.
Chest X-ray, CAT and MRI scan

Chest radiography is an X-ray test that allows doctors to see all the organs in the chest area. Computed tomography or CAT scanning is a test that also uses X-rays and allows doctors to obtain images in the form of cross-sections or in three dimensions.
In turn, magnetic resonance imaging (MRI) is an examination in which doctors obtain detailed images of the inside of the body, in two or three dimensions. Provides much more specific information than radiography or CAT scanning.
If there is a pericardial effusion, there is a change in the shape of the heart, which these tests can detect. Usually, the heart rate increases when more than 250 ml of fluid accumulates in the pericardial sac.
At over 50 ml of fluid, we can talk about pericardial effusion. Therefore, a chest x-ray, for example, does not show an enlarged heart shape, even if the abnormality is present. CAT and MRI scans are much more conclusive.
Quantification of pericardial effusion
There are no universally accepted criteria for quantifying the volume of pericardial effusion. All methods have limitations in determining the actual amount of fluid in the pericardial sac.
The most accepted quantification technique is the one proposed by Weitzman. It is based on M-mode echocardiography. It proposes the addition of echo-free spaces in the anterior and posterior sacs at the end of diastole. It is a slight overflow when the value is 10 mm or less, moderate between 10 and 19 mm and severe when it is 20 mm or more.
It is important to rule out the presence of heart tumors and pericardial cysts before making the diagnosis. In addition, doctors should check for pleural effusion or epicardial fat.